 If you have been in a severe car accident, you could have potentially life-threatening injuries. With severe trauma injuries, bleeding can be severe and hard to stop. This severe bleeding is what causes hypovolemic shock.
If you have been in a severe car accident, you could have potentially life-threatening injuries. With severe trauma injuries, bleeding can be severe and hard to stop. This severe bleeding is what causes hypovolemic shock.
If you have severe enough injuries to sustain hypovolemic shock, you probably have also suffered additional injuries to your spine or extremities. Hypovolemic shock is very dangerous, but once you have stabilized, you will need to find a trusted team that is experienced with car accident injuries to help develop a treatment and rehab plan for any other injuries. As expert car wreck doctors, our team has a comprehensive approach to your injuries and healing.
What Is Hypovolemic Shock?
Hypovolemic shock is a life-threatening condition that occurs when your blood volume drops swiftly and severely. This drop in blood volume means the heart cannot pump enough blood through the body to permeate the tissues and organs. The deprivation of oxygen causes the body’s cells to begin to die. This is an emergency, and left untreated, hypovolemic shock can lead to organ failure and even death.
Hypovolemic shock is usually the result of losing a large volume of blood but can also result from excessive sweating, vomiting, and diarrhea. The hypovolemic shock from blood loss is called hemorrhagic shock. You need to seek medical treatment immediately.
Hemorrhagic Losses
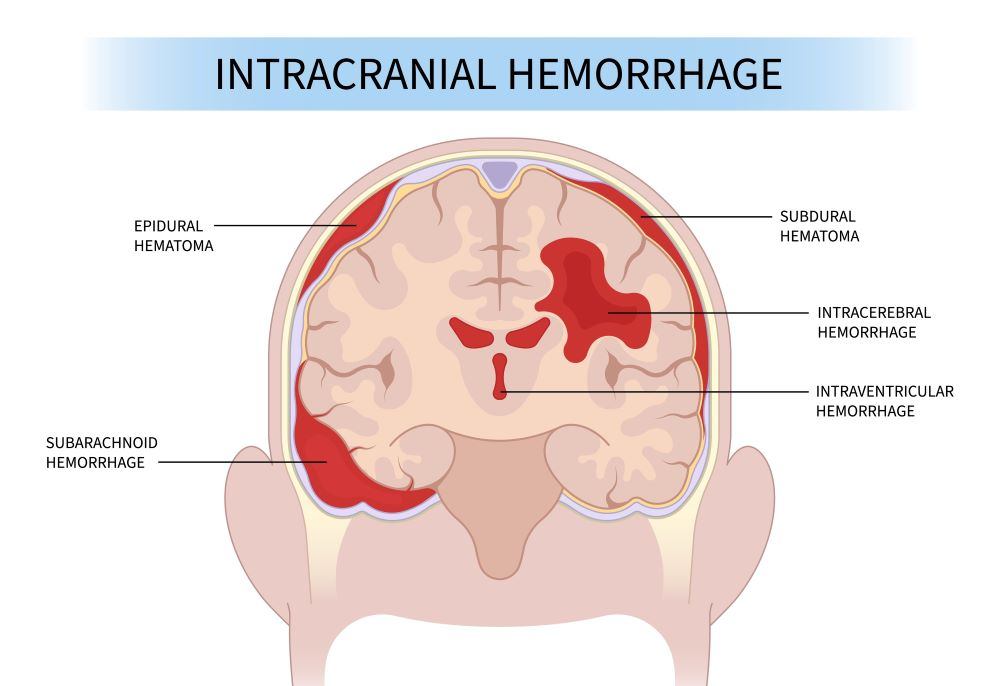
Trauma is the leading cause of death globally, and half of the trauma deaths are due to hemorrhage. Hypovolemic shock can be caused by extreme blood loss. This can occur as a result of open injury, surgical complications, or internal injuries.
A key factor in being able to treat hemorrhagic hypovolemic shock is the ability of the body to clot blood. Since you are losing blood quickly, you are also losing clotting factors in that blood. Without those factors, your blood is unable to slow and clot off. If doctors are unable to catch up on the loss of both blood and clotting factors, your organs will shut down completely and injuries become fatal.
Gastrointestinal Losses
When excessive vomiting or diarrhea happens, your body is unable to replenish its store of fluid in your GI tract. This massive loss of fluid can send you into hypovolemic shock.
Renal Losses
Certain situations like hyperglycemia and dialysis can cause massive salt and fluid loss. This loss can cause your kidneys to begin to shut down and cause hypovolemic shock.
Skin Losses
Your skin is a barrier that helps retain fluids and protect the body. If it is severely damaged, like in the case of massive burns, and leads to hypovolemic shock.
Who is at risk for hypovolemic shock?
Hypovolemic shock affects less than 1 out of every 1000 people and is the most common type of shock seen in children. Any traumatic accident that causes a large amount of bleeding can result in hypovolemic shock. Losing a large volume of fluid from vomiting or diarrhea can affect anyone and result in hypovolemic shock.
What happens during hypovolemic shock?
 As you lose blood volume, your diastolic blood pressure begins to increase. If you continue to lose blood (or fluids), your systolic blood pressure drops. The decrease in blood volume prevents the body from circulating oxygen, and as your body struggles to do this, most perfusion is routed to the brain and heart.
As you lose blood volume, your diastolic blood pressure begins to increase. If you continue to lose blood (or fluids), your systolic blood pressure drops. The decrease in blood volume prevents the body from circulating oxygen, and as your body struggles to do this, most perfusion is routed to the brain and heart.
There are 3 phases of hypovolemic shock that roughly correlate to how much blood volume you’ve lost. The average adult has approximately 5 liters of blood, and it makes up approximately 10% of your body weight.
The Three Phases of Hypovolemic Shock
Phase 1- Compensated Shock
The first phase is the beginning stage of volume loss. Your blood pressure will be elevated, and organ perfusion is still happening fairly well. During this phase, the body’s sympathetic nervous system prioritizes the essential functions of the body and directs blood to the heart, brain, and lungs. This causes a decrease in perfusion to other areas of the body. As the sympathetic nervous system is trying to compensate for the blood loss, the redirection of blood can result in the extremities feeling cold. This is the ideal phase during which the reversal of hypovolemic shock is easiest.
An estimated 15% of your total blood volume has been lost at this point. Despite this, you may still have a normal heart rate and core body temperature.
Phase 2- Decompensated Shock
As your body struggles to compensate and fails to do so, the next phase of hypovolemic shock is called decompensated or progressive shock. Decompensated shock occurs when the body stops being able to compete. This reduces organ perfusion, lactic acid production, impaired oxygenation, and hypotension. These symptoms also coincide with unconsciousness, confusion, and extreme weakness. There is a possibility of reversing shock, but it’s difficult at this point.
Phase 3- Irreversible Shock
This is the most serious phase of hypovolemic shock, and organ failure is inevitable. Tissues and cells begin to die due to the lack of oxygen. Organs begin shutting down, a loss of consciousness is inevitable, and the likelihood of death is high.
The 4 Classes of hypovolemic shock
These four classifications of hypovolemic shock were developed by the American College of Surgeons Advanced Trauma Life Support and are used to identify the degree of blood loss and mental status of a patient.
Class 1
An estimated 15% of your total blood volume has been lost at this point. Despite this, you may still have a normal heart rate and core body temperature.
Class 2
You will have lost, on average, 15-30% of total blood volume. You may be experiencing an increased heart rate and respiratory rate.
Class 3
Blood loss of 30-40% has occurred at this point. The patient will have a significantly increased heart rate and respiratory rate.
Class 4
Over 40% of blood volume is lost at this point. It is very hard for someone to survive this final phase of shock.
What symptoms can indicate hypovolemic shock?
- Rapid heart rate
- Cold extremities
- Agitation
- Lethargy
- Loss of consciousness
- Confusion
- Decreased urinary output
- Rapid breathing
- Increased sweating
- Low temperature
How is hypovolemic shock diagnosed?
 In traumatic cases with catastrophic injuries, emergency and trauma physicians are prepared to look for signs and symptoms of hypovolemic shock. They will be looking for the beginning stages of shock as they stabilize the bleeding. Beginning symptoms can include Increased heart rate, shallow breathing, and cool and clammy skin, beginning on the extremities.
In traumatic cases with catastrophic injuries, emergency and trauma physicians are prepared to look for signs and symptoms of hypovolemic shock. They will be looking for the beginning stages of shock as they stabilize the bleeding. Beginning symptoms can include Increased heart rate, shallow breathing, and cool and clammy skin, beginning on the extremities.
For other types of hypovolemic shock, the key to diagnosing is a thorough history and physical by your doctor. If you believe you are suffering from the beginning stages of hypovolemic shock, please communicate any symptoms to your doctor. These can include vomiting and diarrhea that will not stop or if you regularly receive dialysis.
What tests are used to diagnose hypovolemic shock?
A variety of tests can help doctors evaluate and decide on a course of treatment for patients with hypovolemic shock.
Initial Vitals
The first round of vitals will be taken to evaluate blood pressure, temperature, and pulse rate.
Blood Chemistry
Lab tests will give doctors a large amount of information about where in the process of shock you are. They will order several blood tests, including CBC for blood count, BUN to evaluate kidney function, and even a glucose test to check for hypoglycemia.
Medical Imaging
- CT, ultrasound, or x-ray can be utilized to locate injuries and the source of any bleeding.
- Endoscopy to check for internal or GI bleeding
How is hypovolemic shock treated?
With hemorrhagic shock, the first goal is to focus on controlling the bleeding. Once the bleeding has been stopped or slowed, providers can focus more heavily on replenishing blood. Administering fluids and blood products to help increase blood volume and correct hypotension will also be done. An evaluation of blood transfusions in one trauma center over the span of one year showed more than60% of massive transfusions were used in a trauma setting.
Non-hemorrhagic hypovolemic shock is primarily treated with IV fluids, although, if required, blood products may be used.
What should you do until medical treatment can be provided?
If you or a loved one is suffering from hypovolemic shock, the primary goal is to seek immediate medical treatment. If the patient cannot be moved, you should keep them warm and comfortable until they can be transported to a medical facility. Do not let them drink, as hypovolemic shock cannot be corrected with oral fluids.
Contact AICA
AICA Orthopedics Lithia Springs has a comprehensive approach to recovery. Following diagnostics and initial treatment, our orthopedists will work closely with our physical therapists and chiropractors to develop the best treatment plan for your ideal recovery. If your injuries are severe enough to suffer hypovolemic shock, you will have injuries that are painful and require a long recovery time. Our chiropractors can help alleviate the pain and discomfort you may experience as a result of your car accident.
If you have been in a car accident, please call our office to schedule an appointment with a trusted orthopedic specialist. It is important to find a respected multi-disciplinary team like AICA Orthopedics to ensure top-level care. We are expert car accident doctors and are uniquely qualified to evaluate your injuries and develop an ideal plan to approach your recovery. Contact AICA Orthopedics Lithia Springs, where top-rated physicians are ready for you 24/7 to get you back to a pain-free life.
